There’s so much happening in healthcare recently. I’ll share what I’m paying attention to. and why.
This content is sponsored by Medbridge. Use my link and code DanaStraussDPT for $101 off your annual subscription and unlimited CEUs for a wide range of clinician types. There are many formats for consuming the CEU courses, including live webinars. These meet the requirements many states, like my home state of New Jersey, require be completed each licensing period. I’ve tried several platforms and this is the best by far. 👇
Top of My Mind
The Government Shutdown Ended—The Can is Kicked until January 31, 2026
But not before it broke a record. Democrats didn’t get what they wanted—an extension of the Enhanced Advanced Premium Tax Credits (EAPTCs). This will impact millions of Americans. Since the EAPTCs went into effect, enrollment in ACA marketplace plans has risen from 11 to now 24 million people per the non-partisan KFF. They report that ACA Premium Payment will more than double for 2026. The snip below and linked is for a family of four.
Many will choose not to sign up for coverage because their premiums go up so much. Some healthier people will opt out, which will increase the risk pool of those that purchase the more expensive coverage. And some will choose to go down to the Bronze plan level, which will have its own impacts.
The questions that remain—will they be negotiated back? Can we really give a benefit to millions of Americans and essentially take it away? Here’s KFF’s calculator if you want to check out the impact on prices based on state and income.
Telehealth flexibilities in fee-for-service and Hospital at Home are restored again. But these benefits relying on annual appropriations bills causes stress and confusion every time they are up for expiring.
CMS Released the CY 2026 Medicare Physician Fee Schedule Final Rule
Here are some notable takeaways:
This is the first year of the different conversion factor for Qualifying APM Participants and non-QPs, with QPs seeing a 3.77% increase to $33.57 and non-QPs seeing an 3.26% increase. Keep in mind that these increases reflect a one-year statutory update provided via H.R. 1, which is not part of the typical CMS budget. That made up 2.5% of the update. The .49% budget neutrality adjustment made up most of the rest of the difference, and that’s related to the new efficiency adjustment
CMS finalized the “efficiency adjustment,” which reduced work relative value units (RVUs) by 2.5% for most non-time based services. They were reduced to incorporate workflow and technology improvements. They plan an incremental approach to making these updates.
CMS took site neutrality into their own hands here and again in the Outpatient Payment System (OPPS), out soon in final rule form. In the PFS, they finalized a site of service payment differential. They are changing the way they allocate indirect practice expense (PE) RVUs based on the site of service, and will reduce the portion of indirect PE RVUs tied to work RVUs to half the amount used for non-facility services. This is important because it has the effect of redistributing payments so office-based providers receive higher compensation than in the past (vs. facility-based providers).
They addressed the big problem with skin substitutes and skyrocketing spending. They will now treat them as incident-to supplies rather than biologicals. They will be reimbursed at $127.28 per square centimeter.
They finalized the Ambulatory Specialty Model, a mandatory alternative payment model that puts specialist physicians at risk for cost and quality of care for patients with fee-for-service Medicare who have congestive heart failure and low back pain. About 25% of physicians who manage these patients will be included. It starts in 2027.
Here’s the CMS press release if you want to dig in more on the Medicare Shared Savings Program (MSSP) updates, the Quality Payment Program (QPP), the Medicare Prescription Drug Inflation Rebate Program, and more.
Why all this matters: CMS is pivoting from precedent, addressing site neutral payments and reducing the weight of non-time-based codes. They are effectively increasing reimbursement for non-facility providers and time-based providers (think primary care and behavioral health).
Who will feel the most negative impact? Interventional providers who are part of health systems.
CMS is finding ways to shift reimbursement in the budget neutral Physician Fee Schedule to independent primary care and behavioral health providers.
The incentive for health systems to own specialty practices has also now dropped slightly.
What do you think?
Here’s the Spreadsheet From the Final Rule Addenda to See Impact Per Specialty
Here’s a Few Screenshots:

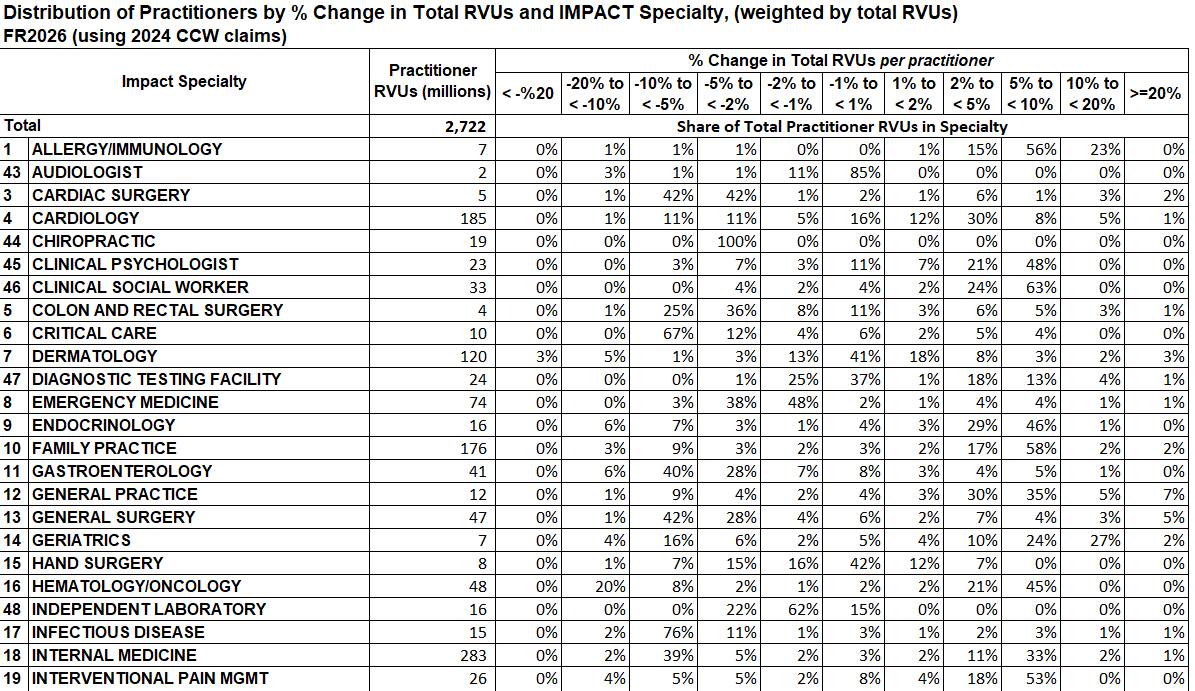
When you look at the impact by specialty, remember this includes both facility and non-facility providers combined. A provider’s actual impacts will depend on whether they are working in a “facility” or “non-facility” site of care.
Here’s the link to the CMS page with all the final rule addenda, which includes the above and the updated Medicare Telehealth List with a few 2026 additions.
What I’m looking forward to next: the Outpatient Payment System Final Rule with the likely finalized removal of the Inpatient Only List and additions to the Ambulatory Surgery Center List. Ambulatory Surgery Centers have instantly become more attractive to those anticipating this and perhaps those looking for new investment opportunities. (More on that in the Resources section below)👀
Participants Announced in the Wasteful and Inappropriate Spending Reduction Model (WISeR):
CMMI launches the WISeR Model in January. The participants are tech innovation companies charged with using artificial intelligence and machine learning, along with human clinical review, to help reduce wasteful utilization of high cost, highly variable procedures in the fee-for-service population.
The model will run in specific Medicare Administrative Contractor (MAC) regions. Providers cannot opt out of authorization for the included services, but can choose whether to request review prior to the procedure or after (which will happen by default if the former is skipped).
Here are the participants selected by MAC region and state:

My take on why this is important:
For the provider types who provide low cost, high value, low variability care, we should welcome this test. The spend included in the unmanaged use of these types of services is gobbling up the budget. Budgets are finite. When spending and frequency of utilization goes up on high cost services, there’s less available for everything else. Conversion factor cuts? Tiny increases? They are the result of managing a budget.
Not to mention that unnecessary procedures performed instead of often efficacious and safer conservative care, when the care is either equally or more effective weighing risks and benefits for that patient, is a safety issue. Less is often more. I’m truly interested in what comes of this model.
I suspect utilization and even requests for authorization to drop in fee-for-service closer to levels seen for these services in Medicare Advantage, partly because providers will be more cautious about whom to recommend these procedures.
Maybe we will see more physical therapist care in place of some of the procedures on the list—and not as a “you have to try this before we do surgery” but instead, positioned to patients as “the evidence tells us that physical therapist care is the best first line treatment for knee osteoarthritis, and here’s why—-. Here are three of the best physical therapists in the region based on their outcomes for patients with knee osteoarthritis. Let us know what information you need to decide on a PT and we will help you secure your appointment today.”
Here’s hoping 🤞
Resources and Other News
Out this week in Health Affairs Forefront, the authors of this piece provide commentary on CMS’ site neutral policy plays in recent annual rulemaking, and rightly point out something for us to keep in mind about the importance of health policy here:
Following the CMS Health Tech Ecosystem?
CMS held a Connectathon on Thursday, November 13, 2026
They showcased progress on their Interoperability Framework and invited those who signed the pledge. Recognize any names of pledge signers? Here are the categories:

Growth of Ambulatory Surgery Centers
There’s an interesting pdf report on private equity in ambulatory surgery centers linked on this site. While the end of the Inpatient Only List will inevitably reduce high cost spend in hospital settings of care, new incentives mean new opportunities that venture capital is already identifying. That will come with its own impacts. Worth a read.
*Disclaimer: All opinions and ideas expressed in this article are solely mine and none represent a recommendation or should be viewed as advisement of any kind to anyone to do anything.*