Top of My Mind
Medicare Beneficiaries are Paying Higher Fee-For-Service Premiums in 2026 | Part B Premiums jump almost 10%
On November 16, 2025, the Centers for Medicare & Medicaid Services announced updated cost figures for Medicare Parts A, B, and D that will take effect in 2026. These annual adjustments are mandated by the Social Security Act.
The monthly standard premium for Part B coverage will increase to $202.90 in 2026, representing a $17.90/9.7% jump from the current $185 rate. Beneficiaries will face a higher annual deductible of $283 for Part B services—$26 more than the 2025 deductible of $257. According to CMS, these cost increases reflect anticipated growth in healthcare prices and usage patterns similar to those observed in previous years.
The CMS Fact Sheet is here. In it, they note this:
The increase in the 2026 Part B standard premium and deductible is mainly due to projected price changes and assumed utilization increases that are consistent with historical experience. If the Trump Administration had not taken action to address unprecedented spending on skin substitutes, the Part B premium increase would have been about $11 more a month. However, due to changes finalized in the 2026 Physician Fee Schedule Final Rule, spending on skin substitutes is expected to drop by 90% without affecting patient care.
If you haven’t followed the astronomical spending on skin substitutes, it’s mind-blowing. And there’s no evidence these treatments are superior to other advanced wound care products. More information is below. Suffice it to say the fee-for-service system leaves patients, taxpayers, payers, and accountable care organizations/value-based care participants vulnerable to harm caused by bad actors’ behavior.
CMS Published the 2026 Outpatient Payment System Final Rule
I’m sharing three of the most consequential takeaways. You might categorize the first two under their “fraud, waste, and abuse” framework of this Administration, and are steps towards their overall goals to reduce unnecessary and avoidable spending. And the third? CMS addresses hospital safety. This falls under the themes of public transparency and accountable care:
The Inpatient Only List is being eliminated over a three year period, beginning with mostly musculoskeletal procedures in 2026. For reference, in 2025, the IPO list has 1,731 HCPCS codes in total. The eliminated procedures may now be done in the hospital outpatient department when deemed appropriate by the physician. In addition, those procedures were also added to the Ambulatory Surgery Center List, allowing flexibility in HOPD or ASC for the site of setting for the procedure. Some may remember that this was finalized at the end of the first Trump Administration and was rolled back under the Biden Administration.
When procedures are removed from the IPO list, hospitals begin to lose dependable reimbursement. For orthopedic surgeons in the coming years, they now have more options. I would expect them to do what they have done in the past with this new flexibility—move more surgeries to the HOPD and ASC settings. Consider the impacts this may have on you and what opportunities and/or risks it may surface. For example, fewer 3-night, hospital inpatient stays will mean fewer discharges to SNFs. Home health and outpatient rehab providers that make home visits? Opportunities!
Like in the PFS Final Rule, CMS is expanding site neutral payment policy reform. For 2026, CMS addresses reimbursement for drug administration services such as chemotherapy infusions. These services will now be reimbursed at the Medicare Physician Fee Schedule rate, which is about 40% of the OPPS rate. Hospitals have long pushed back on site neutral payment policy reform, and a lot of this has been through advocacy at the Congressional level. CMS is showing us here that they have the statutory authority to make some site neutral payment policy changes like they did with the “efficiency adjustment” in the Medicare Physician Fee Schedule (MPFS).
Note: site neutral payment reforms have been endorsed by a wide range of organizations. However, they have faced significant headwinds from acute care hospital advocacy groups. Hospitals are some of states’ largest employers and wield significant influence on the Hill.
Why site neutral payment reform matters right now: This is year one of four of the Trump Administration’s efforts on site neutral payment reform. While Congress itself can make big changes that effectively reduce federal spending to hospitals, CMS itself can make meaningful changes. I wouldn’t be surprised to see this done incrementally over the next few years. Congress could also act, and I wouldn’t count that out, either.
CMS is making an update to the Hospital Quality Star Rating related to hospital safety. Bottom line: they are making it impossible for an acute care hospital to receive a five stars if their safety is in the lowest quartile. For 2026, hospitals in the lowest quartile in the “Safety of Care” group will be capped at four out of five stars. Starting in 2027, hospitals in that lowest quartile will receive a one star reduction, regardless of their overall rating. So a three star hospital, for example, will drop to two stars.
One way hospitals have proactively improved their safety is by embarking on the path to becoming a High Reliability Organization, or HRO. A simple way to imagine an HRO is an organization that prioritizes safety over everything else. Think nuclear power plants and airlines. Those are the OG HROs! Below are the five HRA Principles 👇
Another interesting note on hospital safety and this moment in time: FDA Commissioner Dr. Martin Makary has been sounding the alarm on hospital safety for many years. He has long called for reducing unnecessary procedures and reducing the risk of harm in hospitals. He has also written several books on these and relate topics, all with the theme of calling for reform to protect patients. I’ve listened to his three books on audiobook and my favorite is “The Price we Pay.” His first book, “Unaccountable,” is the basis of the television show “The Resident.”
Here’s a YouTube clip about “The Price we Pay,” which centers around the cost of hospital bills bankrupting Americans and how he volunteered to join patients in court—and was widely successful in those efforts 👇
Congress Remains Divided on an ACA Subsidy Extension as Enhanced Credits Set to Expire on December 31, 2025.
Congress has yet to reach an agreement on how to address the Enhanced ACA subsidies that are set to expire, leaving millions of insured Americans in limbo. Unless Congress acts, nearly 22 million people could see their health care costs dramatically rise or lose coverage altogether.
Republicans have proposed redirecting subsidy funds into Health Savings Accounts or Flexible Spending Accounts, arguing that empowering consumers to shop directly for care would drive down health care prices and increase market competition. However, health policy experts warn that this approach would likely pull healthier, wealthier individuals out of the traditional ACA marketplace, destabilizing the insurance risk pool and potentially triggering a premium death spiral that could collapse the marketplaces altogether.
Here’s an HFMA takeaway from the November 19th Senate Finance Committee hearing if you aren’t up for watching the three-hour recording but would like a quick snapshot.
I see these two facts underappreciated in banter on social media on this topic:
HSAs and FSAs can’t be used for insurance premiums and
Having no health insurance is not a solution. I see a shocking number of healthcare professionals and healthcare consumers fail to appreciate the enormous risk of not being insured for hospital and emergency coverage
Childbirth, accidents, fractures, infections…no one should count out the chance that they may need an emergency room or inpatient hospitalization. Without hospital insurance coverage, you are playing roulette.
Maybe an extension of the enhanced tax credits is the solution or maybe it’s something else. There’s plenty of debate about that. But with a little more than a month from the expiration of current policy, something should be done for the short term, at least.
Additional Links:
KFF’s resource on site-neutral payments is here.
Medicare Payment Advisory Committee (MedPAC) comments on the Proposed Rule earlier this year can be found here, including their perspectives on the above changes I highlighted.
OPPS Fact Sheet is linked here.
Institute for Healthcare Improvement resource on High Reliability is here.
Issue Brief from the Bipartisan Policy Center on the Enhanced Premium Tax Credits here.
Resources and Other News
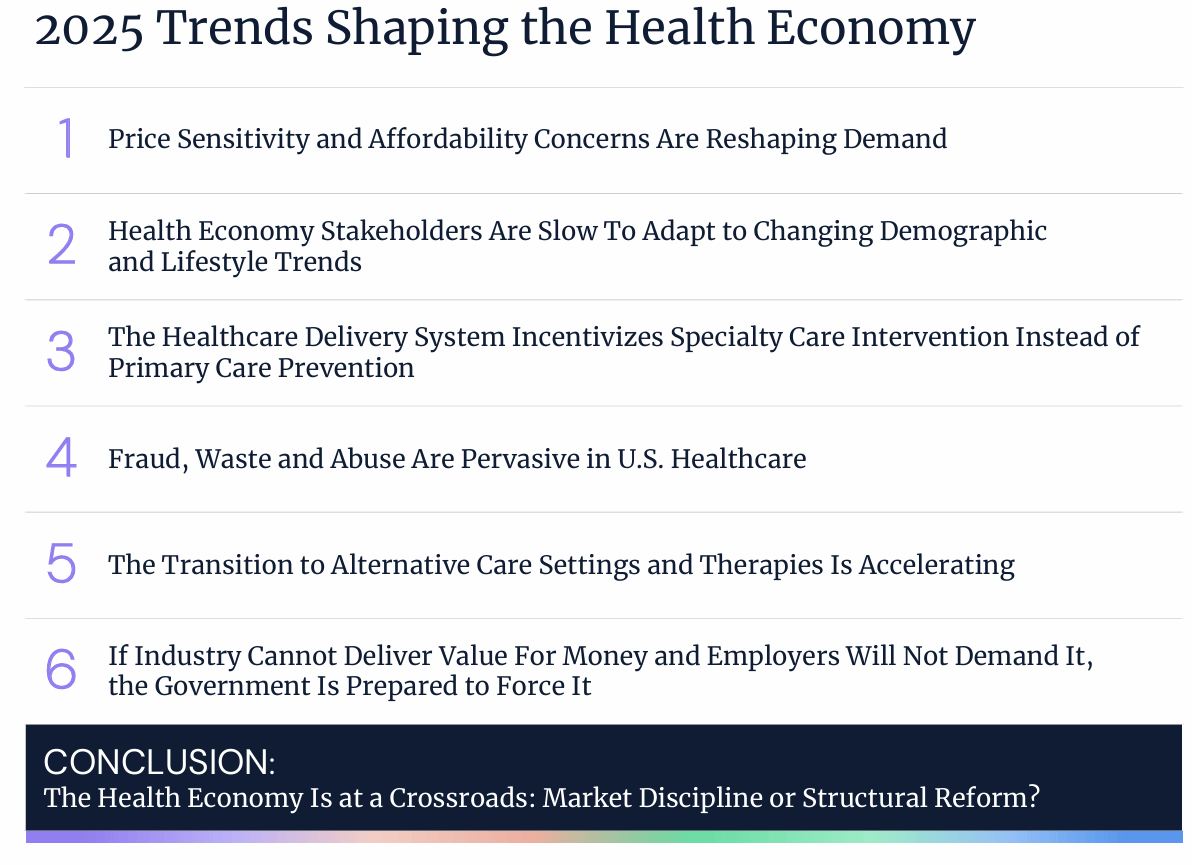
I was listening to this Health Affairs podcast episode called “Why the US Healthcare System is Unwell | Allison Oakes” and they were talking about this Trilliant Health report.
This visual is from page 5:
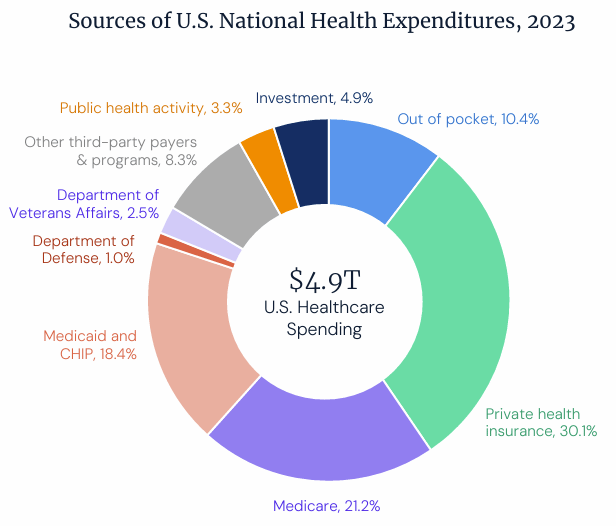
There are some excellent visuals in this piece of content. It’s worth clicking on the pdf even if just to check them out. They stick with you.
They point out six trends they found by analyzing supply, demand, and yield. This is from page 11:
My favorite, from page 35:

From page 41 on pay disparity by physician specialty type (another incentive problem in the American healthcare system. In the report, check out how we differ in percent of physicians in primary vs. specialty care in comparison to other countries.:
Full disclosure—I don’t know Trilliant Health and in an effort to streamlining the process of drafting the newsletter, I didn’t research the organization much. I didn’t want that to stop me from sharing this, but always do your own research on anything I share, of course. 😄
MedPAC Publishes Their 2025 Medicare Payment Policy Resources
This resource is updated for policymakers as they consider Congressional reforms of or changes to Medicare policy.
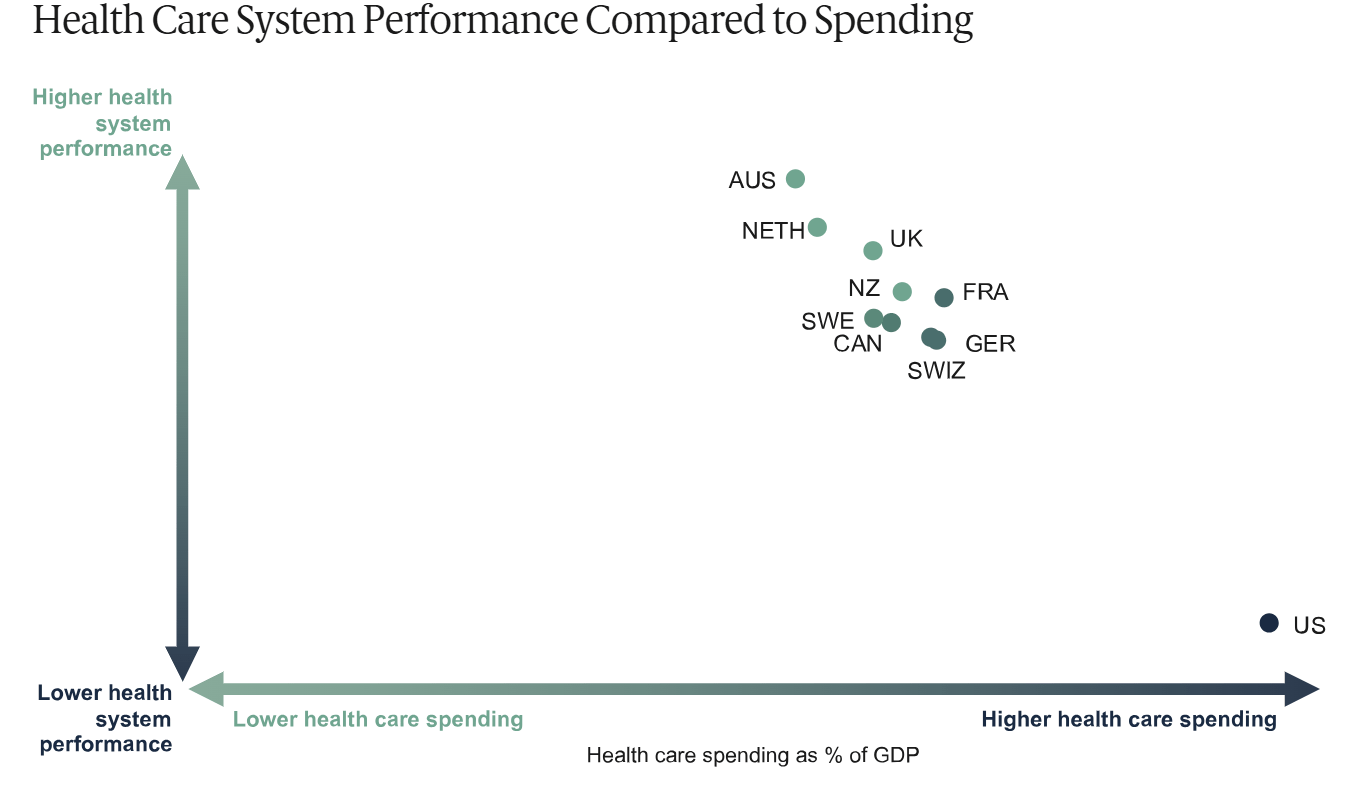
The U.S. Continues to Underperform Nine Peers in Health Care Spending Compared to Performance (2024 Commonwealth Mirror, Mirror Report)
The U.S. is essentially a poor-performing outlier in performance and spending. Old news, but ongoing news. Maybe that’s the biggest takeaway. 👇
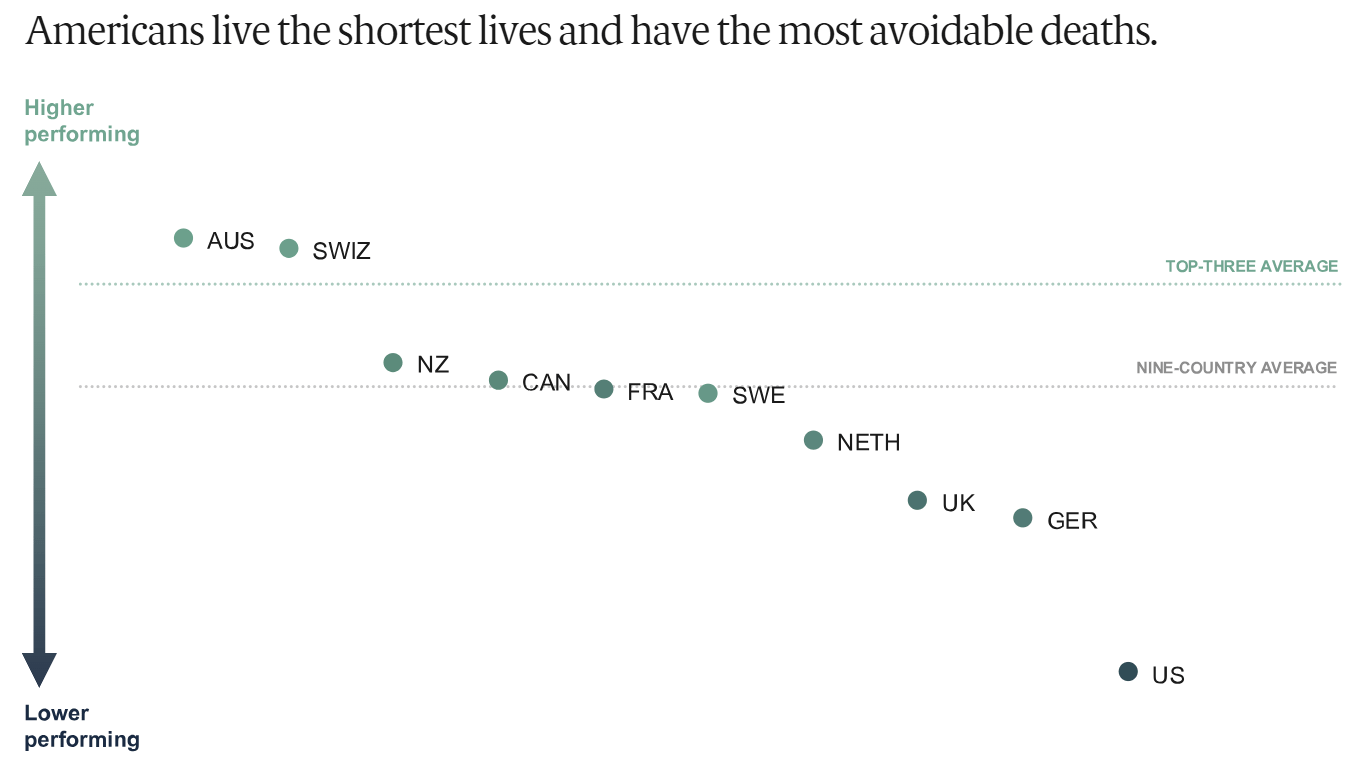
And our lives are worse for it as a whole. It’s awful, stomach-turning stuff, right? 👇
Who has the highest overall ranking? Australia and The Netherlands.
Our problems? They include the below reasons and more:
Poor access to care and affordability—foundational challenges.
A primary care infrastructure in need of strengthening. We don’t invest nearly enough in primary care or optimize the provider types available in primary are settings.
Administrative complexity, which drags down efficiency, adds to burnout, uses up available resources, and more.
Care coordination and integration are very limited, and this leads to overspending, patient harm, lack of patient engagement, and more.
High prescription drug costs, unique to the U.S. vs. our peers. This can have dramatic impacts on those who need brand name and specialty medications, especially those who are uninsured or underinsured
*Disclaimer: All opinions and ideas expressed in this article are solely mine and none represent a recommendation or should be viewed as advisement of any kind to anyone to do anything.*
I co-author the above with Alex Bendersky. Please consider checking it out!