Additional reading by Cody Lee, PT, DPT 👇
**Disclaimer: All opinions and ideas expressed in this article are solely mine and none represent a recommendation or should be viewed as advisement of any kind to anyone to do anything.*
Policy Pulse
Problem/Solution = 20%
We’ve long known that about 80-90% of clinical outcomes are not the result of clinical care. Clinical care is defined here as treating clinical conditions.
Yes, the below are a sampling of factors that have more of an effect on you, your patients, your members, your clients’ clinical outcomes than anything.
Where you live
Health literacy
Income and wealth
Social status
Employment and working conditions
Nutrition and diet
Physical activity, strength, and power
Access to care and social supports
Food environment
Safety
Housing stability
Preventive health behaviors
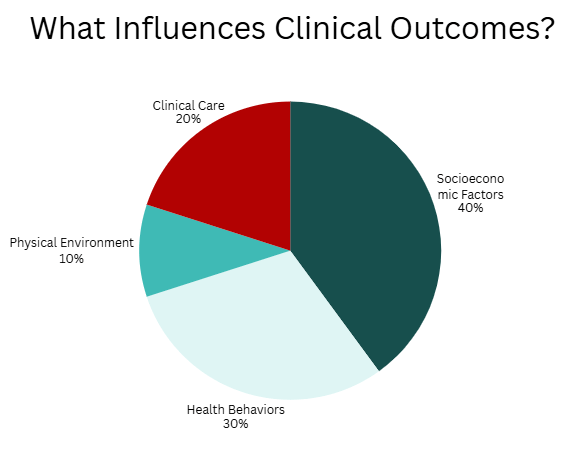
Made with Canva Pro
Let’s step back and think of the role policymakers can and are playing as they consider this reality. The term CMS has been using lately is “evidence-based prevention.”
Talking Out of Two Sides of Their Mouths?
There’s a paradox worth noting here.
On one hand, leadership at CMS and CMMI, like Dr. Mehmet Oz and Abe Sutton, have been talking about and creating programs that fund substitutions in spending to tackle high downstream utilization costs. Models like ELEVATE, ACCESS, and the Rural Health Transformation Program are testing the ability of innovation to address the non-clinical drivers of health outcomes and high spending.
In these and other programs, CMMI is allocating resources to nutrition counseling, partnerships with community-based organizations, funding technology, transportation, etc.
They also want to control what spending is considered “prevention” and which is considered “wasteful social spending.”
On the other hand, CMS has taken three major actions to phase out state-led social determinants of health programs that are trying to accomplish much of the same—address the issues that drive long-term poor outcomes and high costs.
(Note that the below doesn’t even touch on the $1 trillion in Medicaid cuts that begin to be implemented in 2027.)
In March of 2025,CMS rescinded Biden-era guidance that allowed states to use Medicaid to cover housing supports, nutrition interventions, and infrastructure for community health workers. They allow existing state programs to continue until their waivers expire but no new ones will be approved.
In April of 2025, CMS announced it won’t renew Designated State Health Programs (DSHP)/Designated State Investment Programs (DSIP) funding, which is how CMS gave states federal matching dollars for health-related social programs. There are eight states using that funding of about $2.7 billion for programs like California’s housing navigation services, North Carolina’s food-as-medicine pilots, and New York’s nutrition supports.
In July of 2025, CMS blocked the extensions of “continuous eligibility” waivers (keeping people enrolled in Medicaid for 12-24 months regardless of income changes) and workforce development programs training community health workers and primary care providers in underserved areas.
Here are two real-world examples:
North Carolina’s “Healthy Opportunities” program showed $85/month in savings per person through rental assistance and medically-tailored meals. It can’t be renewed.
Massachusetts’ nutrition programs for pregnant women and children was just launched when guidance was rescinded.
How CMMI Funding vs. State Medicaid Waiver Funding Differ
The funding mechanisms for CMMI and the State Medicaid 1115 Waivers are completely different. CMMI spending is capped, and Medicaid waivers are uncapped. However, the policy rationale for their funding is the same. Both are based on a recognition that:
clinical care can only influence outcomes a small percentage
addressing food, housing, transportation, and other factors improves health
“upstream” interventions save money downstream
The other thing to keep in mind is the influence of the executive orders that drove the Medicaid actions, such as rescinding executive orders of President Biden like Executive Order 14009 “Strengthening Medicaid and the Affordable Care Act.”
However, Dr. Oz has said that reasons for changes to Medicaid waivers was budget-related. From the transcript of his swearing-in summary, this was number one of his four priorities as Administrator of CMS:
Eight days before his swearing-in, his agency had announced it would phase out DSHP/DSIP funding (the mechanism that gave states federal matching dollars for programs that address SDOH). The agency stated that these programs were “overly creative financing mechanisms to skirt state budget responsibilities.”
Center for Medicare and Medicaid Innovation (CMMI)
Funded by the Affordable Care Act at the level of $10 billion every ten years. These are not funds that are subject to annual appropriations.
The funding is part of mandatory spending, which has already been authorized by Congress. The executive branch controls how to spend it. In this case, it’s HHS/CMS/CMMI.
There’s no state match required. These are all federal dollars.
There’s no budget neutrality requirement. Models can cost money if they’re projected to eventually save money.
The HHS Secretary and the CMMI Directors decide which models to test
There’s limited judicial review
The Secretary of HHS can expand models nationwide without Congressional approval if the Chief Actuary certifies savings
State Medicaid 1115 Waivers
These are funded through the Federal Medical Assistance Program (FMAP). The federal government matches state Medicaid spending (50-75% match, depending on the state).
The state must match 25-50% of the cost.
They are state driven, so states design, propose, and implement them and CMS approves or denies.
Discretionary approval is required. The waivers are granted at the discretion of the HHS Secretary.
Require renewal every 3-5 years.
What Does This Mean for Private Industry?
The market for “substitute spend” products is still around, but who holds the purse-strings is a consideration.
Keep in mind that if an administration change comes in 2029, “health equity” and state Medicaid SDOH waivers could come back. At the same time, the $1 trillion in Medicaid cuts starting in 2027 are part of a mandatory spending package and will not be easy to rollback. They may also have an impact on these initiatives.
Also, the long-term trend is toward a value-based payment regardless of political administration. What’s nearly unavoidable is that companies that can prove they can reduce total cost of care through non-clinical interventions will thrive under any payment model or whomever is funding the product solutions.
That being said, the market may evolve and bifurcate, where risk-averse organizations adopt lower cost point solutions and “wait and see” approaches, while sophisticated health systems and providers taking full delegated risk from payers may still invest in full-stack platforms. However, they will need to justify them based on diversified value propositions rather than just Medicaid reimbursement.
What is a “full stack” platform for addressing non-medical needs? It’s a company that does screening, intervention, fulfillment, and outcomes measurement.
What is a “point solution” platform? It’s software or a tool that is designed to solve a specific, narrowly-defined problem rather than addressing multiple needs across an entire workflow. They require integration with other systems to support a complete process.
An example of a full-stack platform is Unite Us.
An example of a point solution platform is Aunt Bertha (now called Findhelp).
Integrated Solution or Greater Flexibility and Customization
Regardless of who is funding a product solution, they should be considering this:
Do we want the “elegant” simplicity of one vendor, one platform, one data model? We will have to accept their workflow assumptions, network limitations, and pricing power.
Do we want the flexibility to choose best-in-class tools for each function? We have to accept the integration burden, coordination overhead, and potential data fragmentation.
Might the desire for simplicity, the need to do care coordination, and needing to succeed in value-based payment models push organizations towards integrated social determinant of health platforms?
Might the rapid acceleration in interoperability make it more appealing to choose point solutions?
The Future-Proof Professional
The “substitute spend” trend is becoming an industry norm. It seems like it happened overnight, but it’s here. This is the firewall between health and healthcare cracking. Funding is moving upstream to address what is considered to be the driver of outcomes. As noted above, federal resources via the Innovation Center are pivoting this way while state Medicaid flexibilities are scaled back.
It’s important to recognize this shift and look for opportunities and risks. More on this in Career Moves 👇
Career Moves
Using the Policy Pulse section as a reference, here are three ideas to bridge the gap between policy and your career:
Become a “value navigator.” Clinical and social determinant silos are coming down, and organizations need translators, even if they don’t know it. Learn the language of “total cost of care” and “substitute spend.” If you can frame a non-clinical intervention as a way to prevent downstream utilization and spend, it may strengthen being perceived as a strategic thinker and an asset in a new way.
Bridge the federal-local gap. With state-led waivers facing hurdles, the future may lie in federal innovation models. Position yourself as the person who can identify these federal funding programs and identify potential opportunities.
Master the concept of “full-stack” vs. “point solution.” As organizations choose tools, be able to evaluate them based on value. What solutions may fit better where you work? The “elegant simplicity” of an integrated platform or the flexibility of best-in-class point solutions? Consider what you might recommend based on how these tools solve short-an- long term sustainability vs. solely short-term reimbursement or other solutions.
This Week, Try This
Last week, I talked about my weekly process for managing knowledge and notes that I capture during the week. I shared that I capture to-dos and notes in Apple Reminders and mymind, respectively.
Once or twice per week, I pull up both apps. I decide what belongs in my knowledge management app, Notion.
While I use Notion for many things, one thing I use it for is to collect ideas and content for this newsletter. There is nothing worse than staring at blank page. My capture system helps me hold onto an idea or inspiration or a reference at the moment it hits me, because otherwise, there’s little chance I’ll remember it.
But Notion is where I turn each “capture into something useful.
Here’s a screenshot of a blank version of the database I use 👇

If you want to copy my database template and use it yourself, use this link and then when the site open, click the duplicate button in the top right hand corner.

Click this and the template will duplicate into your own workspace.
If you don’t yet use Notion and still want this database, Notion’s free version has a lot of functionality. When you click the duplicate button, it will take you to this:
A screenshot of the login page that opens when you duplicate a template. If you are using the desktop version already or are already logged in on the web version, it will open immediately when you duplicate it.
Click a “Continue” option and it will set you up automatically and duplicate this template for you.
Let me know what you think! If you like Notion, you can also send any content directly to Notion instead of the Capture step into another app. There’s a chrome extension and a phone app that enable this.
If you try it, let me know what you think!
Thank you for being part of this community. If you enjoyed the newsletter, please share it with a friend!
All the best,
Dana Prommel Strauss, PT, DPT
*Disclaimer: All opinions and ideas expressed in this article are solely mine and none represent a recommendation or should be viewed as advisement of any kind to anyone to do anything.*



