**Disclaimer: All opinions and ideas expressed in this article are solely mine and none represent a recommendation or should be viewed as advisement of any kind to anyone to do anything.**
Love business newsletters? This one’s the OG!
Trusted by millions. Actually enjoyed by them too.
Morning Brew makes business news something you’ll actually look forward to — which is why over 4 million people read it every day.
Sure, the Brew’s take on the news is witty and sharp. But the games? Addictive. You might come for the crosswords and quizzes, but you’ll leave knowing the stories shaping your career and life.
Try Morning Brew’s newsletter for free — and join millions who keep up with the news because they want to, not because they have to.
Policy Pulse
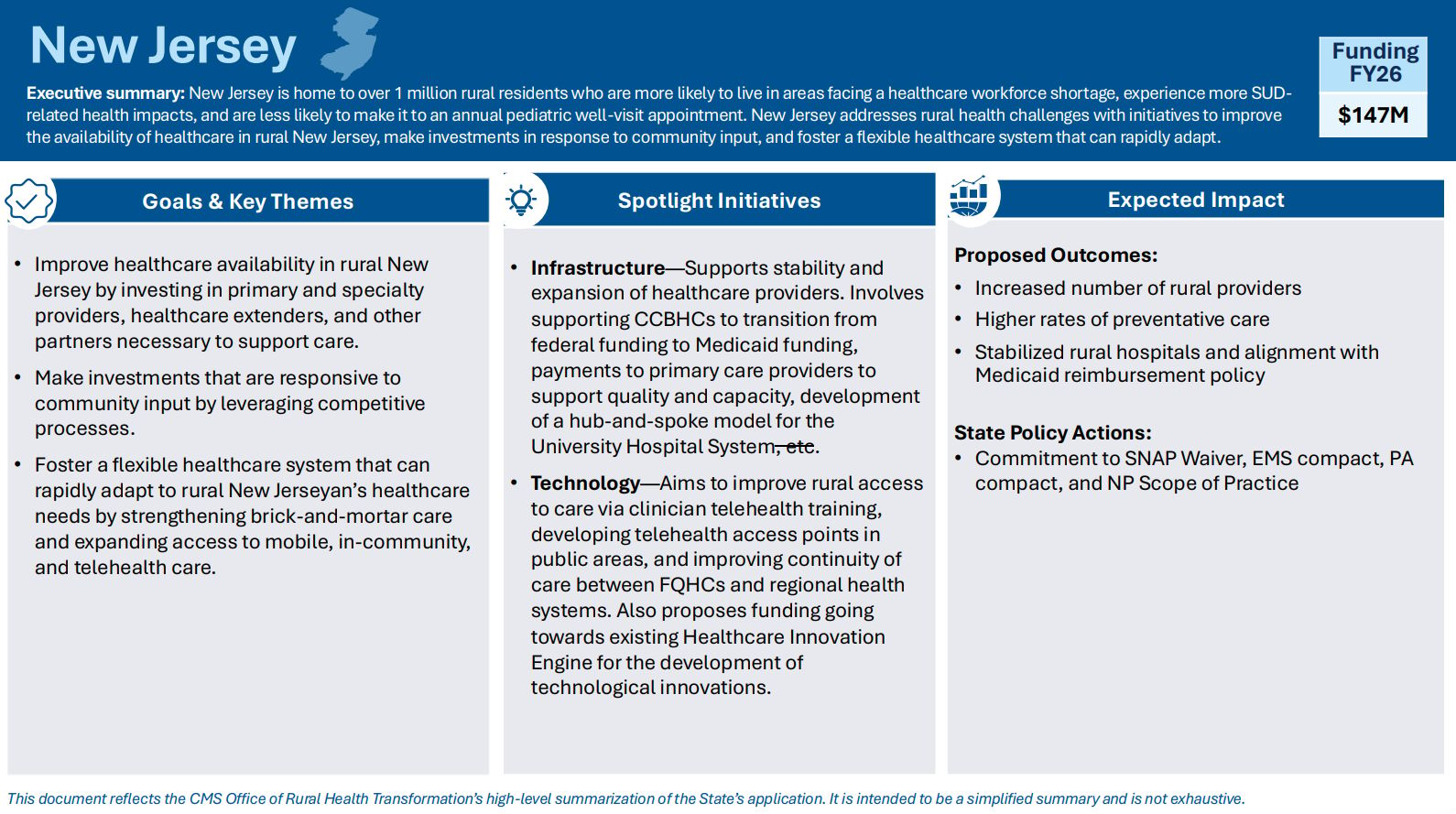
CMS Announces Historic Rural Health Transformation Program
On December 29, 2025, the Centers for Medicare & Medicaid Services (CMS) announced that all 50 states will receive funding from the Rural Health Transformation Program—a $50 billion initiative established under the One Big Beautiful Bill Act (Public Law 119-21) to strengthen healthcare in rural communities.
It’s also thought by many to serve as an indirect offset to funding cuts under that same bill. Supporters believe this innovation funding will pay dividends over time that may be hard to quantify in the shorter term.
The Funding Basics
Total Investment: $50 billion over five years (FY 2026-2030)
Annual Distribution: $10 billion per year
First-Year Awards (2026): Range from $147 million (New Jersey) to $281 million (Texas), averaging $200 million per state
All 50 States Approved: Every state that applied received funding
How Funding is Distributed
The program uses a two-part formula:
1. Base Allocation (50% = $25 billion over 5 years)
Divided equally among all 50 states
Each state receives $100 million annually ($500 million total over five years)
Ensures every state has foundational resources regardless of size
2. Formula-Based Allocation (50% = $25 billion over 5 years) CMS considers multiple factors including:
Percentage of state population in rural census tracts
Proportion of rural health facilities relative to national totals
Status of disproportionate share hospitals
State policy actions that enhance rural healthcare access and quality
Potential impact and scale of proposed initiatives
Other factors as determined by CMS
Important Note: There is NO state matching requirement. States receive 100% federal funding and cannot use these funds to match other federal programs or fill Medicaid budget gaps.
What States Can Fund
States must use funds for three or more approved purposes aligned with CMS's strategic goals. Here are some examples 👇
1. Make Rural America Healthy Again
States can fund evidence-based prevention and chronic disease management programs, including physical fitness and nutrition initiatives, food-as-medicine programs, behavioral health and maternal health services, and expanded access points for primary care.
2. Strengthen Rural Workforce
This includes clinical training programs and rural residencies, loan repayment programs for healthcare professionals, recruitment and retention incentives, career pathway programs, and support for the existing clinical workforce.
3. Modernize Infrastructure & Technology
States can invest in facility and equipment upgrades, telehealth platform expansion, remote patient monitoring systems, cybersecurity improvements, AI tools to reduce clinician burden (including AI scribes), and enhanced data sharing and interoperability.
4. Drive Structural Efficiency
Funding supports hub-and-spoke care models, rural regional centers of excellence, clinically integrated networks, and improved care coordination and resource sharing.
5. Advance Innovative Care Models
This includes value-based care pilots, alternative payment models, regional partnerships and collaboration, and new primary care delivery models.
Key Program Requirements
Oversight & Accountability:
Each state is assigned a dedicated CMS project officer
Annual reports to CMS are required
States must submit regular updates on progress
Annual CMS Rural Health Summit for shared learning
Funds allocated in one fiscal year must be spent by the end of the next fiscal year
CMS may redistribute unspent funds or withhold future payments for fund misuse
There are Some Policy Strings Attached: According to reporting from PBS and other outlets (see “Sources” link at the end of this section), approximately $12 billion of the five-year funding is tied to states implementing "Make America Healthy Again" policies, such as:
Nutrition education requirements for healthcare providers
School participation in Presidential Fitness Test
SNAP benefit restrictions on certain foods
CMS Administrator Dr. Mehmet Oz indicated that funding could be "clawed back" if states don't fulfill promised policy commitments, though he characterized this as leverage for governors rather than punishment.
Context and Criticism
While the $50 billion investment is unprecedented for rural health, it comes alongside significant Medicaid cuts. Key concerns raised by select organizations 👇
National Rural Health Association: Chief Policy Officer Carrie Cochran-McClain noted that while the funding is significant, it won't offset the estimated $1.2 trillion in Medicaid cuts. She emphasized that innovation is difficult when rural hospitals are "struggling to break even" and "concerned about meeting payroll at the end of the month."
American Medical Association: Created a detailed program summary noting the funding is welcome but "will not come close to making up for the estimated $1 trillion in Medicaid cuts" from the same legislation.
Kaiser Family Foundation: Analysis estimates rural areas will lose around $137 billion in federal Medicaid funding over 10 years, far exceeding the $50 billion rural health investment.
What This Could Mean for Healthcare Professionals
The program's structure gives states significant flexibility in how they use funds, which means opportunities will vary dramatically by state. States can allocate funding toward workforce development, infrastructure modernization, prevention programs, and innovative care models—but here’s some of what we don't yet know:
Which states will prioritize which types of professionals in their workforce initiatives
What specific loan repayment amounts, incentives, or programs will be offered
When and how application processes will open
How much funding will reach one type of initiative versus other healthcare priorities
Whether all types of healthcare professionals will be eligible for the same incentives
Some of What We Do Know:
States must use funds for at least three of ten approved activities, which could include workforce recruitment/retention and technology investments
Some states' project abstracts mention musculoskeletal health, fall prevention, and chronic disease management—areas where rehabilitation therapists specifically could contribute, for example
The program emphasizes evidence-based prevention and primary care (which aligns with the scope of practice of primary care focused physicians, behavioral health providers, and rehabilitation therapists)
Infrastructure funding could support telehealth and equipment upgrades for rural clinics
How to Stay Informed
If you are interested in exploring potential opportunities, here are some steps you might consider taking:
Review Your State's Specific Plan: Each state has published project abstracts here. Look for mentions of workforce development and professional-specific plans like musculoskeletal health, fall prevention, or rehabilitation services.
Contact Your State Health Department: Reach out to the agency administering the Rural Health Transformation Program in your state to ask about:
Timeline for funding announcements
Services being prioritized
How to apply for workforce incentives when available
Engage Through Your State Professional Association: Your state association may be or could be planning to advocate for inclusion, for example, in implementation plans and can provide updates on opportunities.
Monitor CMS Updates: CMS will publish state-by-state progress data starting Q3 2026, which may reveal which states are investing in rehabilitation services.
Bottom Line:
The Rural Health Transformation Program represents the largest single rural healthcare investment in U.S. history. While it won't fully offset concurrent Medicaid cuts, it should create significant opportunities for healthcare professionals willing to serve rural communities. Keep in mind there are rural areas in every state!
The program's success will depend on how effectively states deploy resources and whether the funding can drive sustainable improvements beyond the five-year window.
Career Moves
Clinicians often unknowingly limit their career growth by focusing only on growing their clinical skills after graduation.
Here’s what they don’t realize 👇
They may want to grow beyond the role of staff clinician in the coming years.
The longer they postpone other learning, the less it will seem like something they should or could do. And that may make it seem like a career pivot is something that will require another degree or complex career coaching or both.
I have heard countless therapists tell me, for example, “I’d love to do something else, but it’s too late for me,” or “I only know PT—where would I start?”
The truth is that treating clinicians exchange time for money. If they want to do something other than that any time in the future, they must avoid stagnating professionally by focusing solely on clinical skills.
Since wages aren’t keeping up with the financial needs and goals of those with clinical degrees (even those with doctoral degrees like PTs, whose average salary is around $90,000 annually), it simply may not be realistic to remain a staff clinician for your whole career, even if you would prefer to do that.
(Listen to Dr. Eric Makhni, MD, MBA talk about that here.)
So make it an early habit to identify and follow any curiosity about broader healthcare and healthcare-adjacent topics.
-Healthcare economics
-Health policy
-Healthcare quality
-Business operations
-Sales and marketing basics
Where I’d start? Learn how the owner(s) of your company can optimize their financial success. What metrics matter to them and why? What do they likely track on a daily, weekly, quarterly basics? How do their direct reports contribute to their success?
The bottom line from my experience and observation 👇
You can begin to show the potential for competency beyond what you are being paid to do for an employer by starting from a place of knowledge beyond that of a skilled clinician.
So plant the seeds of career growth today! You will not regret it.

From the Notioly Collection
This Week, Try This
First, read your state’s section of the Rural Health Transformation Program State Project Abstracts and your state’s spotlight slide in this deck.
Here’s the slide for my home state of New Jersey 👇
Identify one or two things that interest you.
For NJ, I’m going to look more into the plan for NP and PA scope of practice and whether physical therapists and occupational therapists are included in their plan to invest in improving access to healthcare.
Second, write a brief Linked In post about something that excited you or something you plan to research more.
*Disclaimer: All opinions and ideas expressed in this article are solely mine and none represent a recommendation or should be viewed as advisement of any kind to anyone to do anything.*





